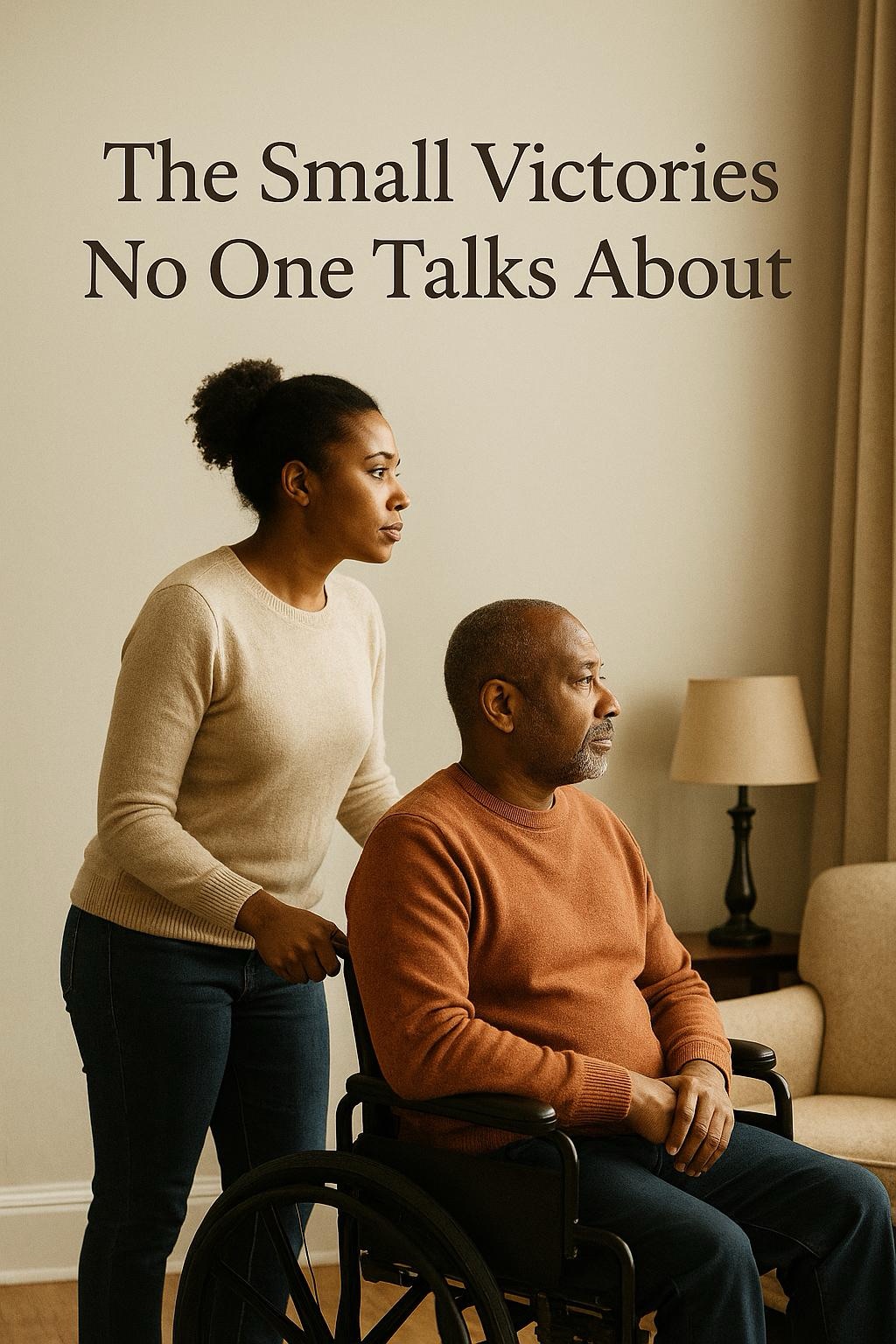
Here he was in physical therapy—taking steps, climbing stairs, walking the full circumference of the large room twice. I was absolutely beaming. I just knew this was the beginning of using the wheelchair only on occasion. He was doing so well, and every session showed real, tangible progress.
Fast forward to today: he can barely take steps, and the wheelchair is now part of our daily reality.
What happened, you might ask?
It’s called insurance.
Anyone who has been a caregiver knows this truth: therapy is like gold. And yet, almost every insurance company caps how much you can receive—no matter how essential it is to recovery.
He was failed from the beginning. The rehab center he was placed in right after his stroke had no therapists on staff, yet that didn’t stop them from billing for therapy services. I reported them, and suddenly outside therapists appeared—but only for 30 minutes a day. That was nowhere near enough. In the meantime, spasticity and atrophy were quietly setting in.
Once he came home, his outpatient therapy was limited to six weeks, twice a week.
By the time his body finally acclimated and began making true progress, the sessions ended—and we were forced to wait until the next year unless we paid out of pocket. At $350+ per hour on a disability income, that simply wasn’t possible.
When therapy ended, he would sink so low. He knew how much it was helping him, and losing that momentum felt like losing hope. Those were some of my hardest moments as his caregiver—watching him slip into discouragement and feeling helpless to change it. I used every bit of reverse psychology, encouragement, and faith I had just to help him keep going.
I rented machines, bought equipment, and tried everything within our means to keep him limber until the next therapy cycle. Even that became expensive. But I stayed positive for him, and leaned heavily on my faith to stay encouraged myself. If our roles were reversed, I know he would have moved Heaven and Earth for me. I simply couldn’t fail him.
What I’ve come to understand is this: stroke recovery is not a sprint. It’s a long, winding journey, and even with the best care, the person will never be exactly who they were pre-stroke.
As caregivers, we can never give up. We are their support, their voice, and their advocates. We do everything we know to do—and then we trust the incredible resilience of the human body. Some things improve with time and determination, and some things simply won’t change no matter what we do.
The key is this:
Celebrate the victories. Don’t drown in what feels like defeat.
In my experience, 75% of stroke recovery is self-determination. If the person you’re caring for doesn’t have the inner drive to keep pushing, your efforts can only take them so far. My husband could have progressed much more if he hadn’t given up when the results didn’t come fast enough. Recovery after a stroke requires grit, resilience, repetition, and a positive mindset—all of which are extremely challenging when depression is part of the equation, as it is for so many stroke survivors.
Today, my husband is wheelchair-bound. His right arm is affected by hemiplegia, and his right leg by hemiparesis. He also lives with aphasia, which limits his speech. That’s a lot for anyone to carry.
But here’s how I keep him encouraged: I point out the victories.
Despite his right side being compromised, he can stand to help me transfer him to the bed, the car, and the bathroom. He couldn’t do that five years ago.
His aphasia has improved dramatically—we can now understand most of what he says. Before, his speech was mostly babble.
He couldn’t write, spell, or text. Now? He can do all three.
He once fixed almost anything around the house but initially did not remember how. Today, he remembers the steps and can direct someone else through the repair. That’s huge.
I’ve witnessed his growth, his setbacks, and his triumphs. And despite everything, I am incredibly proud of him. I look forward to every new victory on this journey.
In my next post, I’ll share ways caregivers can take care of themselves. Most of us deserve a month-long vacation—but that won’t happen for 99% of us. What we can do is take small daily “mini-vacations” to protect our mental, emotional, and physical health. It’s the only way to survive this journey with our sanity and our spirit intact.
Please feel free to share your own story or journey with me. I welcome your questions, your experiences, and your voice. We are stronger together.
Until next time,
Lillian
This blog contains affiliate links. As an Amazon Associate, I earn from qualifying purchases at no extra cost to you. I only recommend products that support caregiving, comfort, and daily living.